The 2016 WHO classification recognized pre-fibrotic primary myelofibrosis (pre-PMF) as a distinct entity. Such knowledge is essential to depict the landscape of pre-PMF and develop mechanism-based approaches to slow the progression of pre-PMF. Here, we conducted a retrospective study of 234 pre-PMF patients defined by 2016 WHO diagnostic criteria in 13 hematooncology centers between 01 January 2015 and 31 July 2023 (ChiCTR2200061208). We evaluated clinical characteristics, risk factors and genetic features of progression to overt-PMF in pre-PMF patients.
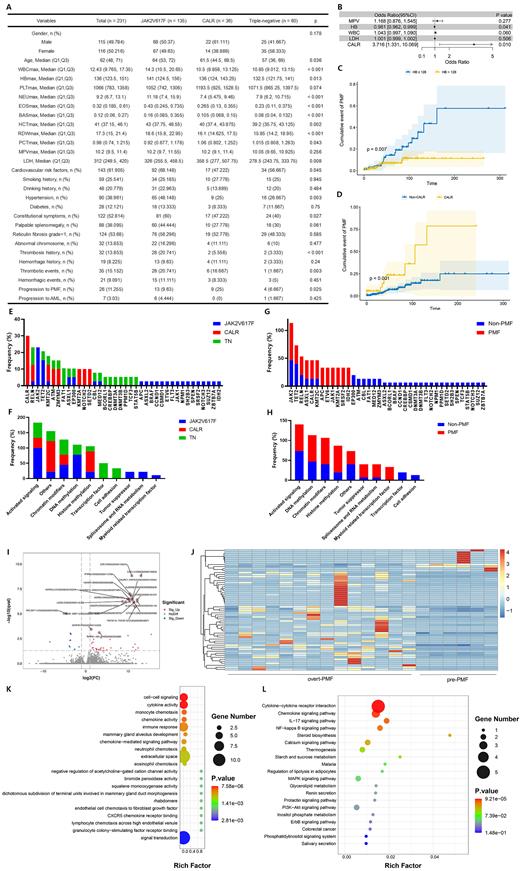
Among 234 pre-PMF patients, 135 (57.7%) harbored JAK2V617F, 36 (15.4%) CALR and 3 (1.3%) MPL mutations; 60 (25.6%) patients were negative for all three mutations. JAK2V617F-mutated patients were older ( P=0.036), had more constitutional symptoms ( P=0.027) and cardiovascular risk factors ( P=0.045), higher white blood cell count (WBC) ( P<0.001), hemoglobin level (HB) ( P<0.001), neutrophile granulocyte (NEU) ( P<0.001), eosinophilic granulocyte (EOS) ( P<0.001), basophilic granulocyte (BAS) ( P<0.001), hematocrit (HCT) ( P=0.002) and red blood cell distribution width (RDW) ( P<0.001) (Figure A). CALR-mutated cases had higher platelet hematocrit (PCT) ( P=0.043) and lactic dehydrogenase (LDH) ( P=0.008). Besides, CALR group had a higher proportion of 25.0% to progress to overt-PMF than JAK2V617F group (9.6%) and TN group (6.7%) ( P=0.025) (Figure A).
As for risk factors of progression to overt-PMF, univariable analysis found it was associated with mean platelet volume (MPV) ( P=0.019), HB ( P=0.027), WBC ( P=0.008), LDH ( P=0.004) and CALR mutations ( P=0.007). Multivariable analysis revealed that lower HB value ( P=0.041; HR 0.981, 95% CI 0.962-0.999) and CALR mutation ( P=0.001; HR 3.716, 95% CI 1.331-10.069) had negative impact on the progression to overt-PMF (Figure B). When divided by HB with cut-off point of 128 g/L, patients with HB value ≤128 g/L were more likely to progress to overt-PMF compared to >128 g/L groups ( P=0.007) (Figure C). And patients carried CALR mutation were also more likely to progress to overt-PMF ( P<0.001) (Figure D).
We performed next-generation sequencing (NGS) in 18 pre-PMF patients, including 9 JAK2V617F, 3 CALR and 6 TN, 3 of which progressed to overt-PMF and 15 stayed in pre-PMF until the end of the follow-up. JAK2V617F was the most frequently mutated gene (9/38, 23.7%), followed by TET2 (7/38, 18.4%), RELN (4/38, 10.5%) and ASXL1 (3/38, 7.9%). JAK2V617F-mutated patients possessed more mutations related to activation signaling pathway ( P=0.025) and DNA methylation ( P=0.033) (Figure F). TN patients possessed more mutations related to transcription factor ( P=0.048) (Figure F). Patients who progressed to overt-PMF possessed more mutations associated with myeloid related transcription factor ( P=0.025) (Figure H). We further performed RNA-Seq analysis in 6 pre-PMF samples and 14 overt-PMF samples. Compared to pre-PMF, overt-PMF showed 49 up-regulated and 13 down-regulated differentially expressed genes (DEGs), of which CSCF3 and CXCL13 were significantly up-regulated (Figure I,J). Gene ontology (GO) functional enrichment analysis showed that DEGs were enriched in cell-cell signaling, cytokine activity, monocyte chemotaxis and chemokine activity (Figure K). KEGG biofunctional analysis showed that DEGs were significantly enriched in cytokine-cytokine receptor interaction, chemokine signaling pathway, IL-17 signaling pathway and NF-kappa B signaling pathway (Figure L).
In conclusion, CALR-mutated pre-PMF patients with HB value ≤128 g/L were more likely to progress to overt-PMF. Genetic analysis found patients with high proportion of progress to overt-PMF tended to possess mutations associated with myeloid related transcription factor. And the upregulation of CSCF3 and CXCL13 may potentially drive the progression of overt-PMF in pre-PMF patients through inflammatory and cytokine related pathways.
Acknowledgement: This research was funded by the Key R&D Program of Zhejiang, No. 2022C03137; Public Technology Application Research Program of Zhejiang, China, No. LGF21H080003; Zhejiang Medical Association Clinical Medical Research special fund project, No. 2022ZYC-D09.
*Correspondence to: Jian Huang, M.D., Ph.D., Department of Hematology, The First Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou 310003, Zhejiang, China. E-mail: househuang@zju.edu.cn
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal